|
Initial
research
As a PhD student at the University of Sydney in 1967
Graeme Clark began to review the available research
to "investigate whether a single or multiple-channel
(electrode) cochlear implant would be possible for the
management of a profound hearing loss." (Clark,
1969: 1)
Since
1970 he has led the research in the Department of Otolaryngology
at the University of Melbourne that has resulted in
a multiple-channel cochlear implant that can provide
significant understanding of speech for severely and
profoundly deaf children and adults.
Inspiration
When Australian otolaryngologist Graeme Clark began
developing the cochlear implant or as it was more commonly
known — the bionic ear — overseas researchers
used an implanted device that had wires leading from
the inside to the outside of the head. According to
Clark this presented too many opportunities for infection.
He believed that the implant should be totally imbedded
and receive information via radio signals rather than
linked to an external source. Other researchers also
had different ideas about where the electrode should
be placed. Some placed it outside the cochlea, others
directly onto the auditory nerve.
| Clark
believed that the electrode should be placed into
the cochlea but could not work out how to get the
electrode inside the tiny spiral without opening
it up. He was inspired by nature to find the solution.
When at the beach he picked up a seashell that resembled
the shape of the cochlea. Nearby was a clump of
wild grass that he pulled a few blades from. As
he twined the blades through his fingers he noticed
that they changed stiffness along their length and
were tapered at the top. Looking at these things
he had the idea of carefully inserting the blade
of grass into the shell until it went almost completely
into the spiral. After this he imagined a bundle
of electrodes of fine, strong and flexible wire
that could be inserted into the human cochlea by
easing around the corners and positioned to correctly
stimulate nerve endings. |
|
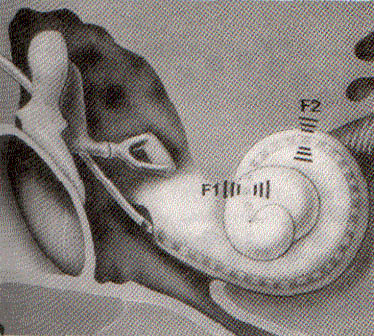
Electrode stimulation pattern resulting
from sound 'ah' (Cochlear Pty Ltd)
|
Resolving
problems
Ethics
Based on the research he had conducted for his PhD,
Graeme Clark and his research team at the University
of Melbourne began fine tuning the design of the implant.
Using Clark's inspiration of the shell and blade of
grass they began to explore the notion of an electrode
array.
As
the
…whole project was still in the research stage,
the Australian team determined to follow the ethical
recommendations made at the Declaration of Helsinki
in 1964 for guiding doctors in clinical research,
as well as the recommendations in the Statement
of Human Experimentation published by the National
Health and Medical Research Council of Australia in
1976. (Epstein, 1989: 44)
As
animal experimentation was needed before the implants
could be used on humans there were also animal ethics
to consider.
For
more information on animal ethics:
Animal
Ethics Committees Manual of Policy and Procedures, The
University of Melbourne, March 1996
Technical
considerations
Some of the problems the research team had to overcome
included:
- the
electrode bundle had to be precisely manufactured
- the
materials needed to be resistant to body fluids and
harmless to the recipient. Clark and his team used
Teflon® coated platinum wires as electrodes to
fit in the cochlea. The multi-electrode array successfully
passed into the cochlea. To resolve the problem of
finding materials resistant to body fluids the designers
looked to work being done on the pacemaker implant.
It was originally cast in epoxy resin, however the
cochlear implant researchers believed a metal may
offer lightness and body fluid resistance. Pure titanium
was trialled for the casing by G. A. and L. Harrington.
G.
A. and L. Harrington was the first company to "deep
draw titanium in Australia. In this process which
requires special expertise, sheet metal is turned
into the required shape with a high depth to width
ratio." (Epstein, 1989: 48)
- the
feedthrough wires had to be insulated - high alumina
ceramic was selected. The Ceramic Corporation Pty
Ltd, specialists in precision industrial ceramics
were approached. The owner, Miroslav (Mirek) Kratochvil
emigrated to Australia as a political refugee from
Czechoslovakia, developed a new ceramic which was
fired at a much higher temperature than normal to
give the properties needed.
- welding
the parts together. A new alloy was developed and
trialed. These three components ensured
…a hermetically sealed implant, completely resistant
to body fluids. …These discoveries were to have
an enormous influence on the development of the Australian
bionic ear, for the electronics to be used in the
implant would also need the protection which only
the hermetic seal devised for the pacemaker could
give. (Epstein, 1989: 49)
- tests
had to be done to determine how to best reach the
cochlea in surgery.
- clinical
trials and selection of suitable recipients had to
be carried out. These trials have influenced current
procedures as well. An effective service network was
an essential ingredient to ensure that the innovation
would fulfil a user's needs.
- the
implant would need to last a long time — a design
life of 70 years.
Funding
the research
Funds were needed to continue the project. Funding was
donated by Melbourne Apex Club, a telethon organised
by Sir Reginald Ansett and Channel 0, The National Health
and Medical Research Council and Lions Clubs International
and at a later stage the Deafness Foundation of Victoria.
Distribution
clinics, an innovation too
The success of the Cochlear implant is founded on a
world wide network of dedicated clinics. At these clinics,
the Cochlear implant is implanted by a surgeon. More
importantly, each recipient is trained by an audiologist
to recognise speech using the system. Training is needed
to recognise the unfamiliar sounds generated by the
speech processor. Try to recognise the nursery rhyme
in this simulation of processed speech.
|
Each
system is customised to suit the individual and
fine-tuned to convey the maximum amount of speech
information. Regular repeat visits ensure that
the system is operating at its peak.
The
success of the Cochlear implant system rests on
careful selection of appropriate patients, reliable
technology, and a network of clinics staffed by
highly skilled surgeons and audiologists.
|
 (Cochlear
Pty Ltd)
(Cochlear
Pty Ltd) |
Developing
a prototype of the cochlear implant
The receiver-stimulator in the prototype device needed
…the
equivalent of 6000 radio valves to make it work, a
sheer impossibility until the development of integrated
circuit technology when that same amount of electronic
circuitry could be condensed into a tiny microchip.
(Epstein, 1989: 43)
The
receiver-stimulator was designed and manufactured by
Melbourne University's Department of Electrical Engineering
and Department of Otolaryngology.
A
prototype receiver-stimulator with a connector for
10 channel electrodes, all to be implanted, and the
University of Melbourne was able to lodge an application
for patent rights. The device was called Umdolee (University
of Melbourne Departments of Otolaryngology and Electrical
Engineering).
The
gold box multiple electrode device measured 4.2 x
3.2 x 0.85 to 1.3cm. It included a sandwich of three
razor-thin substrata and the thousands of transistors.
The electrodes themselves consisted of a bundle of
twenty fine wires, each insulated and fine as a human
hair, the diameter of the whole bundle being about
0.5 mm. This bundle had to replace the work of some
20 000 to 30 000 nerve fibres in the normal ear and
transmit sound impulses to the brain. …each pair
of electrodes controlling a sound of a different pitch.
(Epstein, 1989: 43)
The
speech processor, however, had not been developed. This
was the device to break speech into meaningful signals
that the brain could recognise. The strategies to teach
someone how to recognise speech could only be developed
when a person who had received an implant worked with
engineers and audiologists.
Finding
the first patients
To ensure testing was rigorous and accountable, assessments
for selection of patients and monitoring implantees
was carried out in a multidisciplinary centre featuring
specialists in:
- phonetics:
the study of speech sounds and their production
- audiology:
the diagnosis and rehabilitation of hearing loss
- auditory
physiology: the physiology underlying normal and impaired
hearing, speech and language in humans. Physiological
measurement techniques are used to identify and assess
hearing impairment.
- information
science: the collection, organisation and analysis
of data.
- otology:
the diagnosis and treatment of disorders of the ear.
- psychophysics:
how electrical stimulation by the cochlear implant
is received by the user and how best to present speech
information to them.
- psychology:
patient support and family counselling.
- psychoacoustics:
conducts basic and applied hearing research specifically
aimed at understanding and correcting impaired hearing.
- speech
rehabilitation: re-establish speech patterns.
- electrical
engineering support: identify and modify hardware
and software problems.
Once
the prototype was developed and extensive animal testing
proved satisfactory the device was ready for implanting
in a human. Rod Saunders received a ten channel implantable
device in 1978. The surgery was a success and Rod heard
his wife speaking to him after the device was turned
on.
For
a more detailed history of the cochlear implant:
http://www.medoto.unimelb.edu.au/info/history2.htm
and for a History of the University of Melbourne/Cochlear
Limited Cochlear Implant
http://www.medoto.unimelb.edu.au/info/history3.htm
|